Due to the World Health Organisation’s (WHO) currently elevated status as a result of the COVID-19 pandemic, now would be a perfect time to gain a better understanding of what the organisation is and what it does. This article will look at the inner workings of the WHO, what its role in global governance is, and how it is funded.
Established in 1948 upon the signing of its constitution, the WHO currently works across 150 countries and, throughout its history, has been lauded for its many successes.1 Some of those successes have included its tireless efforts to vaccinate children, resulting in the elimination of smallpox in 1979, its successes in reducing polio infections by 99%, and its steadfast leadership when responding to the 2002-2003 SARS epidemic.2 Presently, the organisation is headed by former Ethiopian health-minister Director-General Tedros Adhanom Ghebreyesus who began his five-year term in 2017.3 The organisation is also guided by a World Health Assembly (WHA), comprising delegates from all 194 member states who determine policy and budget, and an Executive Board of technically qualified members who implement the decisions and policies put forward by the WHA.4 5
The WHO states that its primary role is to ‘direct and coordinate international health within the United Nations system’ with its main areas of focus being on the advocating for universal healthcare, the tackling of non-communicable and communicable diseases, and the ability to prepare, survey and respond to public health risks.6 7 Over its lifetime, the role played by the WHO in global health governance has changed and prior to the 2002-2003 SARS outbreak, it was relatively limited in what it was able to do. Action taken by the organisation were contained to the management of international borders and the enforcement of requirements by governments to monitor the spread of a small selection of infectious diseases. The SARS crisis was largely influential in the decision to reform and expand the organisations in 2005. With these reforms came revised International Health Regulations which expanded the remit of the WHO and introduced the ability to authorise the issuing of a Public Health Emergency of International Concern (PHEIC) (using both official and unofficial information to do so). The WHO also issued ‘best practise’ guidelines to national and subnational authorities, and the monitoring of pandemic preparedness of national health systems. The new reforms also set out to improve domestic health systems in general and the networking between them across borders.8
The declaration of a PHEIC is the highest level alert the WHO is able to declare. It signifies to countries the need to combat the spread of disease, mobilise resources, and to fund research and development on treatments, vaccines and diagnostics. During a PHEIC, countries are obliged to share information with the WHO and, whilst non-binding, the organisation is also able to announce travel and trade restrictions, as well as treatment guidelines designed to prevent the implementation of economically harmful restrictions.9 Since its introduction, a PHEIC has been declared during the 2009 swine flu epidemic, twice as a result of Ebola in 2014 and 2019, in reaction to the resurgence of Polio in 2014, and finally, as a result of the Zika virus outbreak in South America in 2016.10 In the month between the WHO being informed of COVID-19 by China on 31st December 2019 and the declaration of a PHEIC on 30th January 2020, the organisation had begun to post guidance, vet and distribute diagnostic tests worldwide, and begin supply-chain management in an attempt to ensure all countries would have access to the necessary equipment.11 Once the PHEIC had been announced, strategic preparedness and response plans were initiated with the WHO initially asking for $675 million from its donors in order to implement them.12
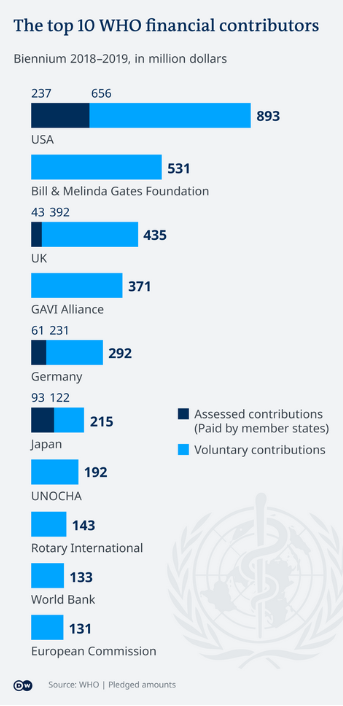
Whereas the WHO is able to directly control the 20% of its budget taken from dues, the other 80% is given in voluntary contributions with instructions attached to ensure the money goes towards specific initiatives and projects of the donors’ choosing.20 This greatly limits the WHO’s capacity to effectively conduct operations due to it largely being at the whim of its donors, resulting in a loss of autonomy as the organisation becomes greatly receptive to the demands of its member states. This is largely why the WHO was so reluctant to criticise the Chinese government’s response to the COVID-19 outbreak as, although currently not a significant donor, the Chinese have increased their contributions by 52% since 2014 and have the potential to become a major donor.21 Further to this, whilst the USA is increasingly looking inwards, China is looking to continue to expand its economic and political influence across the world. China has formed meaningful coalitions with lower-income countries through their ‘Belt and Road initiative’, and are therefore currently seen as a more prudent investment by the organisation.
Throughout its history the WHO has proved an integral component to global health governance, acting as a focal point from which responses and initiatives are able to be coordinated in times of health crisis. However, like any multi-national organisation reliant on its members for funding, the WHO is a greatly political organisation and as such has to perform a constant balancing act in order to survive and to get the most from its members – both in terms of finance and cooperation.

